As a pediatrician in Beverly Hills, I see children and families every day—and one of the most alarming trends I’m witnessing is the rising use of vaping devices and nicotine pouches among adolescents. While much attention has been paid to cigarette smoking in past decades, a new generation of nicotine delivery systems is quietly sneaking into our homes, our teens’ social circles, and unfortunately, their brains.
In this post, I’ll speak in plain language about why vaping and nicotine pouches are a serious concern, what the data show, and how you as a parent in Beverly Hills can act proactively to protect your child’s health.
Why I’m Concerned
I’m trained to watch for risks to children’s health—from well-child checks through adolescence. Nicotine, the core addictive substance in many of these products, is especially dangerous for developing brains. A well-documented scientific fact: Nicotine exposure during adolescence can disrupt brain development, leading to long-term effects on attention, learning, and emotional regulation.
When a device promises no smoke, or a pouch promises “smoke-free” nicotine, it may feel less threatening—but make no mistake: The danger remains real.
What Are the Products at Issue?
Vaping devices (e-cigarettes): These heat a liquid (often with nicotine, flavorings, other chemicals) and produce a vapour inhaled by the user.
Nicotine pouches: These are small sachets, placed between the lip and gum, that release nicotine without burning tobacco. They are marketed as “smoke-free,” “tobacco-free,” and often with appealing flavors.
Both are being used increasingly by young people, and both carry addiction and health risks.
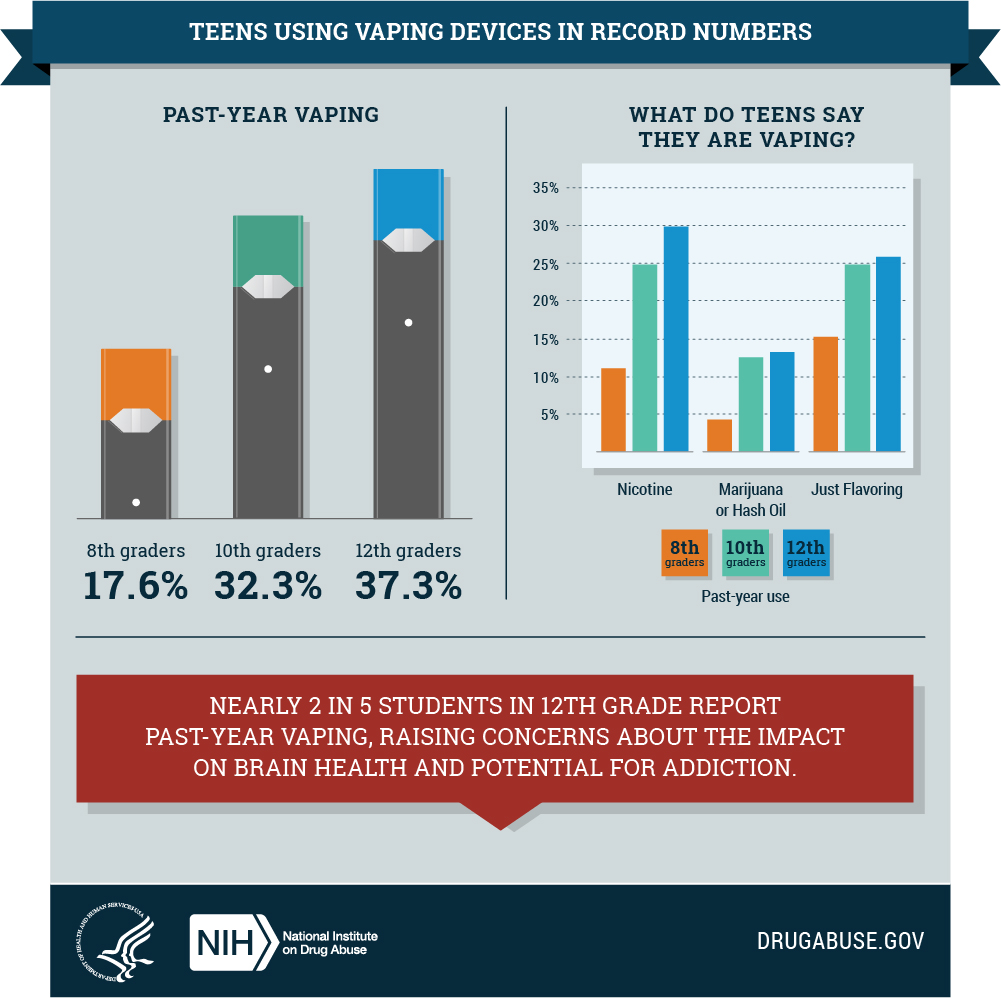
What the Data Show
Here are a couple of critical data points that all parents should know:
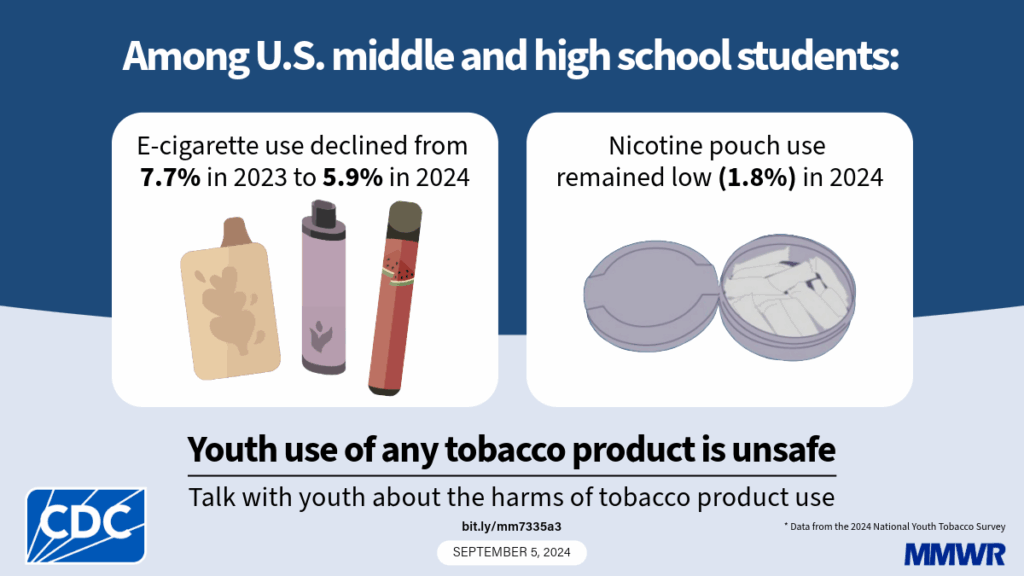
- According to the Centers for Disease Control and Prevention (CDC), in 2024 nicotine pouches became the second most commonly used tobacco product among U.S. youth (middle and high school students), at about 1.8 % current use. (CDC)
- A recent study found that for children younger than 6 years old, the rate of unintentional ingestion of nicotine pouches increased by 763 % from 2020 to 2023. (STAT)
In other words: not only are older kids using these products, but younger children are accidentally exposed and harmed because of these quieter nicotine formats.


How These Products Work in the Body
When a teen uses a vaping device or a nicotine pouch, nicotine enters the bloodstream and affects brain receptors responsible for reward, memory, and impulse control. Because adolescent brain development continues into the early 20s, introducing a powerful stimulant like nicotine can derail healthy development.
Here is one scientific fact you should know: The adolescent brain is far more susceptible to addiction because the “reward” circuits mature before the “control” circuits. In short, teens are biologically primed to form nicotine addiction more easily than adults.
Why This Is Especially Relevant for Beverly Hills Parents
Living in Beverly Hills means you’re in a community where resources are strong—but it also means children have broad access to social opportunities, peer influence, and high-pressure settings (academics, social media, sports). That combination can create vulnerability to “safe-looking” products like vaping devices or nicotine pouches masquerading as harmless.
Here are things you should watch for:
- Flavored or sleek nicotine pouches hidden in backpacks or sports bags.
- Social media posts showing teens using discreet “lip pouches” or vaping in bathrooms or hidden areas.
- Teens who claim they are “just vaping for flavour” or “just using a pouch every now and then” — the “just” is what gets them into trouble.
- Signs of nicotine dependence: irritability, mood swings, difficulty concentrating, needing to use a device/pouch during study breaks or social events.
The Real Health Consequences
Beyond addiction, what are the health impacts?
- Respiratory issues: There is increasing evidence that vaping is associated with lung irritation, inflammation, and in some cases, hospital‐treated lung injuries.
- Oral health problems: Nicotine pouches placed between lip and gum can promote gum recession, irritation, and may increase risk of lesions.
- Cognitive and emotional effects: Adolescents using nicotine show higher levels of anxiety, difficulty focusing in school, and increased risk of using other substances. For example, one study noted that nearly 40 % of teens who vape report frequent use. (Truth Initiative)
- Unintended poisoning: As noted earlier, the sharp rise in accidental ingestion among young children underscores how dangerously accessible these pouches are.
What Parents Can Do — My Friendly Advice
Let me offer some straightforward steps you can take right now:
- Open a conversation
Sit down with your child and ask neutral, supportive questions: “I’ve heard that vaping and lip pouches are showing up among teens. What’s your take on it?”
Use a friendly tone, rather than an accusatory one. This helps them feel safe sharing rather than hiding. - Educate with facts
Share the data: for example, “In 2024, about 1.8 % of middle/high school students reported using nicotine pouches” and “Accidental ingestion of pouches by kids under six increased over 700 % in recent years.”
Provide the scientific basis: Nicotine harms developing brains. - Check the environment
Take a look around your home: what devices or containers could be concealing nicotine pouches? Are there snacks, bags, or sports kits where a pouch could be placed?
Discuss the risks of exposing younger children with older siblings, babysitters, and caregivers. - Set clear boundaries
Communicate your expectations: “We expect you not to use any nicotine device or pouch. If you have questions or temptations, come talk to me before trying.”
Establish consequences and help them understand why—not just rules, but health reasons. - Encourage healthier alternatives
If your teen is feeling stressed due to school demands or peer pressure, help them find healthy outlets, such as sports, arts, peer groups, and mentoring. Create ways for them to manage stress without turning to nicotine. - Stay informed about new products
Technology and marketing move quickly. Pouches, discreet vapes, and flavored nicotine products are evolving. Stay up to date with trusted sources, such as the CDC or peer-reviewed studies. - Model the behavior
If you use nicotine or vaping, consider quitting—or, at least, discussing openly with your child about why you are doing so and how difficult it is. Honesty builds trust.
Why It’s Urgent
Even if the use rates of some products are starting to decline in older teens, the emergence of nicotine pouches remains a significant concern. While the 1.8% figure for pouch use may seem small, consider this: that is nearly half a million youth in the U.S. alone. (Monitoring Tobacco Product Use) And every early nicotine exposure increases the risk of long‐term addiction and health issues.
For a community like Beverly Hills, the stakes are high—not because our children are less vulnerable, but because the opportunity and peer networks are more complex. The “silent” nature of pouches and vaping (no smoke, often discreet) make them harder to detect and easier to rationalize (“just this once,” “just at a party”).
A Final Word From Me
As a pediatrician, I already counsel families about nutrition, sleep, vaccine schedules, screen time, and mental health. I now find myself spending more time than ever on the topic of nicotine in its modern forms—vapes and pouches. I don’t write this to alarm you, but to arm you—with facts, strategies, and the community support you need so your child can thrive without the hidden trap of nicotine.
Our children deserve to grow up in a safe environment—where they can learn, play, dream—and not be sidetracked by an avoidable addiction. You can make a difference by staying informed, staying present, and staying connected to your child.
For more information or to schedule a consultation, please visit my practice page at BeverlyHillsPediatrician.com.
Let’s work together to keep our children healthy—today and for their whole future.
— Dr. Anita Sabeti
References & Further Reading
- CDC: “Youth Tobacco Product Use at a 25-Year Low, Yet Disparities Persist.” (CDC)
- Tobacco Free Kids: “Awareness and Use of Nicotine Pouches.”
- National Institute on Drug Abuse (NIDA) on youth vaping trends.
- For deeper research:
https://truthinitiative.org/press/press-release/significant-drop-youth-e-cigarette-use-marks-progress-nearly-40-teens-who-vape
https://assets.tobaccofreekids.org/factsheets/0427.pdf
Thank you for trusting me with your child’s health. Let’s keep the dialogue open.
